Yes, research shows that youth with ADHD have more trouble sleeping and that problems sleeping make symptoms of ADHD, and other aspects of daily life, worse. Fortunately, treatment options, including behavioral interventions, supplements, and prescription medications, can offer children and adolescents with ADHD some relief from sleep difficulties.
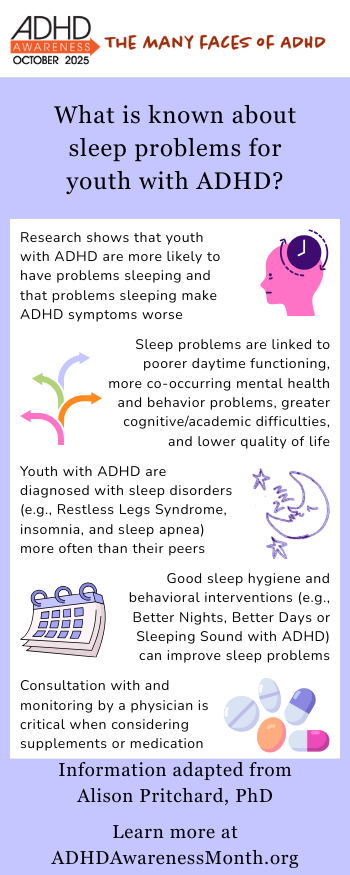
Research shows a bidirectional relationship between sleep and ADHD in children and adolescents. That is, youth with ADHD are more likely to have problems sleeping AND problems sleeping make symptoms of ADHD worse. Conservative estimates suggest that between ¼ and ½ of youth with ADHD are impacted by sleep problems, and both longitudinal and experimental studies have shown that sleep problems actually cause poorer daytime functioning in youth with ADHD.
Children who have difficulties with sleep are more likely to have both more severe ADHD symptoms and more co-occurring mental health and behavior problems. Additionally, sleep problems are associated with greater cognitive and academic difficulties and with lower quality of life for youth with ADHD.
Children and adolescents with ADHD experience a broad range of sleep-related difficulties. They are more likely than children without ADHD
- to have trouble falling asleep,
- to wake in the middle of the night,
- and to have trouble waking up in the morning.
- They resist going to bed,
- move more in their sleep, and
- are sleepier during the day.
Teenagers with ADHD tend to take longer to fall asleep, sleep less overall, and spend more time awake during the night. It’s not a surprise, then, that youth with ADHD are diagnosed with sleep disorders, like Restless Legs Syndrome, insomnia, and sleep apnea more often than their peers.
Options for treatment
Fortunately, there are some options for treating sleep problems in youth with ADHD. Of course, good sleep hygiene is essential, but may not be enough to meaningfully improve sleep in these children. Behavioral interventions for sleep are a good option when improvements to sleep hygiene aren’t sufficient. These interventions often involve identifying the specific nature of the child’s sleep difficulties and working with a clinician like a psychologist or pediatrician to learn and practice strategies to address those difficulties.
Two behavioral interventions that were specifically designed for and tested with youth with ADHD are: Better Nights, Better Days, and Sleeping Sound with ADHD. Both have been shown to improve sleep problems among kids with ADHD.
If sleep problems persist despite good sleep hygiene and behavioral interventions, then supplements or prescription medications may be necessary. While melatonin is commonly used, there is relatively little research on its effectiveness and parent perceptions of its utility vary widely. Similarly, there are only a small number of studies evaluating the effectiveness of prescription medication (e.g., clonodine) that is sometimes used to treat sleep problems in children. Consultation with and careful monitoring by the child’s physician is critical when supplements or medications for sleep are being considered.
About the Author

Alison Pritchard, PhD is a child and adolescent clinical psychologist at Kennedy Krieger Institute and an Associate Professor at Johns Hopkins University School of Medicine. Her clinical and research interests center around attention-deficit/hyperactivity disorder (ADHD) in childhood and adolescence, with a particular focus in sleep.
References and Links
- Teen Sleep Toolkit
- Sleep Strategies for Kids
- Wajszilber D, Santiseban JA, Gruber R. Sleep disorders in patients with ADHD: impact and management challenges. Nat Sci Sleep. 2018;10:453-480. doi:10.2147/NSS.S163074
- Becker SP, Epstein JN, Tamm L, et al. Shortened Sleep Duration Causes Sleepiness, Inattention, and Oppositionality in Adolescents With Attention-Deficit/Hyperactivity Disorder: Findings From a Crossover Sleep Restriction/Extension Study. J Am Acad Child Adolesc Psychiatry. 2019;58(4):433-442. doi:10.1016/j.jaac.2018.09.439
- Bondopadhyay U, Diaz-Orueta U, Coogan AN. A Systematic Review of Sleep and Circadian Rhythms in Children with Attention Deficit Hyperactivity Disorder. J Atten Disord. 2022;26(2):149-224. doi:10.1177/1087054720978556
- Lunsford-Avery J, Carskadon M, Kollins S, Krystal A. Sleep physiology and neurocognition among adolescents with Attention-Deficit/Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatry. Published online 2024. doi:10.1016/j.jaac.2024.03.005
- Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in Children With Attention-Deficit/Hyperactivity Disorder: Meta-Analysis of Subjective and Objective Studies. J Am Acad Child Adolesc Psychiatry. 2009;48(9):894-908. doi:10.1097/CHI.0b013e3181ac09c9
- Lunsford-Avery JR, Krystal AD, Kollins SH. Sleep disturbances in adolescents with ADHD: A systematic review and framework for future research. Clin Psychol Rev. 2016;50:159-174. doi:10.1016/j.cpr.2016.10.004
- Larsson I, Aili K, Lonn M, Svedberg P, Nygren JM, Ivarsson A, Johansson P. Sleep interventions for children with attention-deficit/hyperactivity disorder (ADHD): A systematic review. Sleep Medicine. 2023; 103:64-75. doi: 10.1016/j.sleep.2022.12.021